What is
Asthma? Children under 5
with symptoms Is your Asthma
well-controlled? Asthma Triggers
and how to avoid Asthma Treatments
and how to use devices How to use
inhalers and devices What do to in
an Asthma attack Allergic Rhinitis –
triggers and avoidance Instructional booklets,
leaflets, flyers and videos
Did you know?
- It is estimated that 1 in 5 children and 1 in 10 adults have asthma.
- Asthma is common, distressing, disabling, misunderstood, life-threatening and TREATABLE!
- YOU CAN lead a full, active, unrestricted life with asthma:
- No coughing, wheezing, tight chest or shortness of breath.
- No waking at night.
- No time off school or work.
- No more visits to the Emergency Room.
- No admissions to hospital.
- Huge savings in healthcare.
- Full participation in all activities, including sports.
What is Asthma?

Asthma is a condition that affects the airways – the small tubes that carry air in and out of the lungs.
- If you have asthma your airways are extra sensitive.
- When you come into contact with something you are allergic to, or something that irritates your airways (a trigger), your airways will become narrower, making it harder to breathe.
- The muscles around the airways tighten. The lining becomes inflamed and swollen. Sticky mucous if often produced.
Symptoms of Asthma
- Coughing
- Wheezing
- Shortness of breath
- Tightness in the chest
Not everyone will get all of these symptoms. Asthma varies from day to day, person to person and may come and go throughout your life.
Diagnosis of Asthma
Diagnosing Asthma in adolescents over the age of 12 years and adults
Asthma is a disease which is extremely variable and therefore not always easy to diagnose. Your symptoms may be intermittent or persistent, they may vary over time and intensity.
Step 1
- if you have a cough, wheeze, chest tightness and shortness of breath you should see you doctor.
- Your doctor will ask if anyone in your family has asthma, allergies, eczema or food allergies.
- Your doctor will ask whether you have gastric reflux, whether you are taking a medication which may cause a cough, what your occupation is as you may be exposed to potential triggers, which are causing your symptoms. Obesity may also be causing these symptoms.
- Your doctor will listen to your chest and may take a peak flow measurement.
- Ideally a lung function test (Spirometry test) will be done however since the start of the pandemic these have stopped due to the risk of spreading the coronavirus. A normal spirometry test does not mean you do not have asthma as you may not have symptoms at the time of the test!
Step 2
- Your doctor may do a simple reversibility test using a peak flow meter before and after using a bronchodilator inhaler. Or may ask you to see an Asthma Nurse educator, who can help you monitor your own symptoms at home.
Step 3
- Your doctor may prescribe an asthma inhaler – the preferred treatment following Global Guidelines 2023 (GINA) for adolescents and adults over the age 12 years is a combination inhaler (Budesonide and Formoterol. This may be used daily as a preventer medication and as a reliever inhaler. This is called SMART therapy).
- The correct diagnosis of asthma is not always made after one appointment and follow up is very important. You may be referred to a pulmonologist for further testing such as FeNo (fractional exhaled nitric oxide) if necessary.
Diagnosing asthma in Children from 6 to 12 years
Almost half of all young children under the age of 5 years cough and wheeze usually whenever they get a cold and may be prescribed inhalers – this does not mean they will have long term asthma.
You pediatrician will take a detailed family history, as asthma runs in families. They will ask if anyone in the family has asthma, allergies, eczema or food allergies.
Premature babies are more likely to cough and wheeze with viral infection in the first 5 years.
If your child has eczema and food allergies and you have a family history, these are the children who are more likely to have long term asthma.
You pediatrician my start treatment with 1 or 2 inhalers - Global Guidelines (GINA) 2023 recommend a low dose preventer inhaler daily until diagnosis confirmed or taking a reliever inhaler with a preventer as needed.
Why did I get asthma?
ANYONE can have ASTHMA – young, old, men, women, athletes, artists, ANYONE!
Asthma can start at any age. Some people get symptoms during childhood, which may come and go throughout life. Others develop ‘late-onset’ asthma in adulthood, without ever having had symptoms as a child.
It is unknown for sure what causes asthma. What we do know is that:
- Genetic – asthma is more likely if there is a family history of asthma, eczema or food allergies and environmental allergies such as rhinitis.
- Lifestyle - Many aspects of modern lifestyles - such as changes in housing and diet and a more hygienic environment - may have contributed to the rise in asthma over the last few decades.
Smoking during pregnancy increases the chance of a child developing asthma symptoms.
Click here for flyer.
Caring for children with Asthma
Children UNDER 5’s
Almost half of all young children under 5 will cough and wheeze at some time, usually when they have a cold or viral infection and many will be prescribed inhalers.
Click here for flyer.
Which children are more likely to be diagnosed with asthma?
Children with a family history of:
- Asthma or allergies
- Eczema
- Food allergies
Premature babies are more likely to cough and wheeze with viral infections in the first few years, but are more likely to have ongoing asthma after the age of 5 if they have - a family history of asthma or allergies, eczema or food allergies.
Children exposed to cigarette smoke, even before they are born, are more likely to cough and wheeze and be admitted to hospital with breathing difficulties in the first 5 years.
Triggers - the most common trigger in children under the age of 5 is colds and viral infections. Children in daycare or nursery may get 10 colds a year, therefore those children with asthma symptoms must be treated.
Medications for UNDER 5’s:
Asthma symptoms (cough, wheeze and a tight chest) are difficult to treat in children under 5 years. Their airways are tiny and giving inhalers is difficult. As soon as children can use a spacer with mouthpiece the better – most children by the age of 4 years can use a spacer with mouthpiece with their medications.
Medications
Step 1: Quick reliever inhaler - Ventolin or Airomir (usually blue) - 2 puffs given for cough or wheeze as prescried. NEVER LEAVE HOME WITHOUT IT!
Step 2: If symptoms persist a controller medication may be prescribed. Either - a controller inhaler Flixotide (orange) or Beclomehtasone (Becotide) usually brown - (given every morning and evening even when your child is well) This takes 7 to 10 days to be effective. OR Singulair (once daily from 6 months given as sprinkles in applesauce & chewable tablets from the age of 2 years).
Steroids - a short course of Oral steroids may be prescribed for acute asthma episodes.
Spacers - help more of the medicine get in the airways. As soon as children can use a spacer with mouthpiece the better. Medications then reach the small airways and asthma will become easier to control. See an asthma nurse to learn how to use spacers effectively.
What else can I do to help?
- Have plenty of fresh air and physical activity and swimming is good for lung development.
- Blow bubbles and pinwheels
- Encourage a good diet with plenty of fruits and vegetables.
- Have plenty of physical activity to help the lungs develop.
Is your Asthma well-controlled?
Take control of your Asthma.
- See your doctor annually – make sure you have the RIGHT diagnosis and the RIGHT treatment.
- Call an Asthma Nurse – get asthma education.
- Talk with your pharmacist.
- Know how and when to take your inhalers.
- Have a Personal Asthma Action Plan – learn how to recognize when your asthma is getting worse.
(Feel free to download form and take with you to annual doctors visit.)
- Know what to do in an acute asthma episode (Asthma Attack)
- Avoid your triggers.
Asthma Triggers and how to avoid
An Asthma Trigger is anything that irritates your sensitive airways and may cause asthma symptoms.
It is impossible to avoid all triggers, but avoiding as many as possible will help you control your asthma.
Viral infections (cold and flu)
- Wash hands regularly
- Open windows to improve ventilation especially in nurseries and classrooms
- Get the flu shot annually.
Allergens - such as dust-mites, mold, pollen, grasses, animal dander and cockroaches.
- Replace pillows every year.
- Do not have carpets in your home, wood or tile floors are much better.
- Encourage your child not to have too many soft toys – place in freezer every week for 6 hours to kill the dust mites.
- Wash bed linen in hot water weekly.
- Allow your bed to air before making it.
- Visible mold must be treated with diluted Bleach, any cracks in the ceilings or wall must be repaired.
- Do not bring Easter lilies into your home.
- Do not have pets in your bedroom.
- Cockroach infestation must be treated by a professional pest control company. Try to keep food in the kitchen and dining areas only and clean up after meals.
Irritants - such as household cleaning chemicals, air-fresheners – sprays and plug-ins and essential oils, perfume, paint, varnishes and smoke from cigarettes or open fires.
- Do not use household chemicals either aerosols or sprays. Try to clean using microfiber cloths, a steam-cleaner and a vacuum cleaner with a HEPA filter.
- Do not use air fresheners, plug ins or essential oils.
- Open windows to encourage good ventilation.
- Do not allow smoking in your home.
The weather – high humidity, extreme cold, thunderstorms and hurricanes.
- There is little we can do about the weather!
- When humidity is very high use an air-conditioner ensuring that filters are cleaned regularly.
- In extreme cold weather when overseas wear a scarf over your nose and mouth.
- Hurricanes means blinds will be closed, electricity lost, fans and air-conditioners cannot be used, the air becomes stagnant and hot resulting in indoor mold. Outside debris will be flying, leaves falling, excessive rain will encourage mold to grow in abundance. Be prepared to adjust asthma medications to avoid flare up. Keep calm as anxiety will only make asthma symptoms worse.
Exercise – this is often called exercise induced asthma however a better term is ‘exercise induced bronchoconstriction’, this is because the tightening and narrowing of the airways is not caused by having asthma. Many people who experience asthma symptoms only when they exercise may simply have poorly controlled asthma. Some people who experience exercise induced asthma are elite athletes doing strenuous exercise especially in very cold conditions.
- An acting short bronchodilator inhaler, such as Ventolin before exercising may be prescribed.
- If someone is exercising more than 3 times a week it may be better to take a daily preventer or combination inhaler and short acting bronchodilator only if necessary, during or after exercise.
Asthma Treatments and how to use devices
Asthma treatments/medications are safe and effective.
There are two main kinds of asthma treatments:
Controllers/Preventers

Controller inhalers stop your airways from being so sensitive.
They may take 7 to 10 days to be effective.
The protective effect builds up over several weeks.
It is important that you take your controller every day to keep your asthma away!
Relievers/Rescue

Quick reliever inhalers are taken to relieve asthma symptoms
(cough, wheeze & tight chest).
They quickly relax the muscles surrounding the narrowed airways (within 5-10 minutes), making it easier to breath again.
If you need your reliever inhaler more than twice a week, talk to your doctor - you may need a controller inhaler.
This is because reliever inhalers do not reduce the swelling in your airways.
NEW TREATMENT - SMART therapy

How to take inhalers and devices
Asthma UK has created an excellent resource with regards to how to take inhalers and devices.
Please use this link to access ‘how to videos’ regarding your particular inhaler device.
Link to UK videos :
www.asthma.org.uk/inhalervideos
Using a spacer with your inhaler can increase the effectiveness and efficiency of medication reaching the lungs where it is most needed. Approximately 90% of people using spacers are using them incorrectly.
What to do in Asthma attack
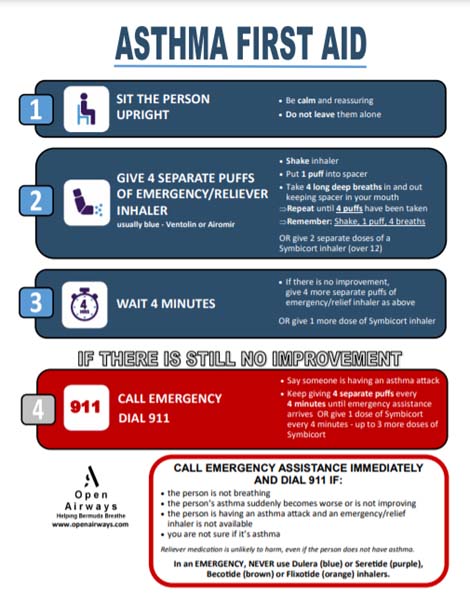 Sometimes, no matter how careful you are about taking your asthma medicines and avoiding your triggers, you may find that you have an asthma attack often associated with a viral infections or flu.
Sometimes, no matter how careful you are about taking your asthma medicines and avoiding your triggers, you may find that you have an asthma attack often associated with a viral infections or flu.
Remember children under 2 years are difficult to treat as airways are very small and medications are difficult to give effectively.
Signs of an asthma attack -
- Coughing incessantly, quick reliever/emergency inhaler not helpful.
- Short of breath.
- Tight Chest.
Severe attack -
- Lips and finger tips turning blue.
- Can’t speak in sentences.
GO TO EMERGENCY NOW!
Allergic Rhinitis – triggers and avoidance
Allergic Rhinitis, sinus allergies or ‘asthma of the nose’, as it is sometimes called, is very common and left untreated makes you feel tired, exhausted and sometimes it is difficult to concentrate.
Allergic Rhinitis should be treated every day during the season when you have symptoms and year-round if necessary.
Many people with allergic rhinitis develop asthma at some time during their life.
Who is likely to develop Allergic Rhinitis?
The tendency to have allergies is often hereditary, although allergies to specific substances are not, as these are acquired by exposure to the irritant. Allergic rhinitis and other symptoms of allergy usually develop by age 10 and peak in a person in their early twenties; allergies often become less severe or disappear in older adulthood.
What are the symptoms of Allergic Rhinitis?
Symptoms vary, but can include:
- Runny nose (clear nasal discharge)
- Itchy, bloodshot, or runny eyes
- Irritated nose or throat
- Nasal congestion
- Sneezing
- Blocked ears
- Dark circles under the eyes
- Trouble breathing.
Treatment options
Antihistamines
Claritin is safe and effective and lasts 24 hours.
It is available without a prescription and does not make you feel drowsy. Claritin D also has a decongestant and may help until you get your rhinitis well controlled.
Zyrtec - On prescription in Bermuda is safe and effective and lasts 24 hours. It is not supposed to make you feel drowsy however, some people do complain of drowsiness while taking it.
Phenergan, Benadryl and Piriton are all non prescription antihistamines. Will make you drowsy so should only be taken at night.
Other treatment options
Singulair once a day prescription treatment.
Unfortunately Singular is not effective for everyone.
Preventative prescription nasal sprays
Avamys, Alestin, Flixonase, Nosacort, and Rhinocort are available in Bermuda.
A safe topical steroid must be used every day during the season when you have symptoms.
Click here for flyer.



